-
Publish Your Research/Review Articles in our High Quality Journal for just USD $99*+Taxes( *T&C Apply)
Offer Ends On
Jeerawan Phakaew*, Pornthep Sirimahachaiyakul and Jintana Rittharomya
Corresponding Author: Jeerawan Phakaew, Department of surgery, Faculty of Medicine Vajira Hospital Navamindradhiraj University, Thailand.
Received: December 12, 2024 ; Revised: December 24, 2024 ; Accepted: December 27, 2024 ; Available Online: December 30, 2024
Citation: Phakaew J, Sirimahachaiyakul P & Rittharomya J. (2024) The Effectiveness of Pressure Injury Care by Negative Pressure Wound Therapy. J Nurs Midwifery Res, 3(2): 1-9.
Copyrights: ©2024 Phakaew J, Sirimahachaiyakul P & Rittharomya J. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Views & Citations
Likes & Shares
Pressure injuries are one of the most common complications in patients with impaired mobility and limited movement. They cause illness, increase healthcare costs, and can lead to further complications from pressure injury. Wound care is complex, difficult, and costly. Currently, there are various methods of wound treatment, and negative pressure wound therapy is a popular treatment method. This case study aims to study pressure injury care's effectiveness using negative pressure wound therapy. The case study focuses on a 75-year-old Thai female patient diagnosed with a fracture of the left femur neck, infected grade 4 bedsore, and sepsis. Using a case study report model, the researcher studied the patient over four months (June-September 2022). Data was collected, and nursing problems were assessed using Gordon's 11 health patterns as a conceptual framework for assessment and nursing care planning. The issues identified included the wound not healing within a reasonable timeframe, requiring frequent dressing changes due to contamination with excretions, high material costs for wound care, and patient pain during dressing changes with no visible improvement in the wound. Consequently, the wound care method was switched to negative pressure wound therapy. Results: The wound healed rapidly, and the wound cavity became shallower. The number of dressing changes decreased, reducing the workload and time spent on wound care. Costs were reduced, and patient discomfort during dressing changes was minimized. Conclusions: negative pressure wound therapy is an effective method for healing pressure ulcers, reducing costs, alleviating staff workload, and decreasing patient pain from dressing changes. Both the patient and healthcare staff were satisfied with the outcome.
Keywords: Pressure injury, Negative pressure wound therapy, Wound therapy
BACKGROUND
Pressure injuries, also known as pressure sores, damage patients and health systems. Despite medical advances, the incidence of pressure ulcers has increased slightly in recent years. According to reports, the worldwide prevalence of pressure ulcers is 12.8%, with a hospital-acquired pressure ulcer incidence (HAPI) of 8.4% [1]. Pressure injuries are a complication that increases pain. Increased risk of infection, Prolonged hospital stay, and a decreased quality of life. Joseph [2] from the study found that Pressure ulcers can increase the length of hospital stay by up to 5 times (National Pressure Ulcer Advisory Panel (NPUAP), European Pressure Ulcer Advisory Panel (EPUAP) and Pan Pacific Pressure Injury Alliance [3]. Body positions the most common are the sacrum (28-36 percent), heel (23-30 percent), and coccyx. (17-20 percent) [4]. Studies have shown that negative pressure wound therapy (NPWT) can improve wound healing [5]. This method involves treating wounds with a closed system at a pressure below atmospheric pressure, which is both continuous and discrete. NPWT works by creating a negative pressure environment that promotes wound healing. This is a method of treatment that is popular today. Fleischmann W [6] and colleagues reported this wound-healing method 1993 from a study of diabetic patients with chronic foot ulcers. It was found that dressing the wound using a vacuum (VAC dressing) can reduce the number of times and the time needed to make the wound. It makes the wound heal faster. The wound is more minor than the wet dressing wound, helping to improve the patient's quality of life [7]. It is effective in terms of Reducing wound surface, depth, and degree of granulation tissue formation [8]. From such information, ET nurses, the experts in wound care, ostomy, and bowel control, put their knowledge into practice. Their practice not only promotes wound healing but also Reduces the pain from dressing wounds, demonstrating their empathy and care for the patients, resulting in a better quality of life, shorter hospital stays, and Reduced costs.
OBJECTIVE
To study the effectiveness of pressure injuries care using negative pressure wound therapy.
METHOD
STUDY RESULTS
Case study information
Thai female patient, 75 years old, slim build. There was a history of losing control and falling three months before coming to the hospital. After falling, she had a problem with pain and bought over-the-counter painkillers to take on her own three days before coming to the hospital. There was so much pain that she couldn't move. She had a grade 4 pressure sore on the coccyx and a fever, so she came to the hospital. The doctor diagnosed a fractured neck of the left femur with infected pressure injury grade 4 with sepsis on June 22, 2022. The patient felt fine when admitted-a grade 4 pressure injury on the coccyx, with a foul odor. First, vital signs are Body temperature 38.5 degrees Celsius, pulse 82 times/min, breathing 20 times/min, and blood pressure 138/72 mmHg. The blood oxygen value was 98%. The doctor prescribed bedsore debridement at the coccyx because there was much dead tissue. The patient has underlying diseases, including diabetes, high blood pressure, and gout.
Behavioral patterns, health behaviors Evaluated according to Gordon's 11 health patterns
Physical examination: Elderly patients’ Symmetrical figure, dark skin color, warm skin, has level 4 pressure sores on the coccyx and other bone areas. There are no wounds and no peeling of the skin.
Diagnosis: Infected Pressure sore grade 4 at coccyx.
SUMMARY OF SYMPTOMS AND TREATMENT RECEIVED
Dressing the wound in the first stage is essential because the wound is infected. The culture of the wound revealed the infection. So, the wound was treated by wiping it clean with cotton and gauze moistened with saline (0.9%NSS; normal saline). Wipe the wound and then use gauze moistened with povidone-iodine (1%povidone iodine), which is a substance that destroys or inhibits the growth of microorganisms. It can prevent infection and treat infected wounds [9]. Please put it in the wound and cover it with large gauze (Gamgee). The wound is treated two times a day, but the wound will be changed when the patient has urine or feces on the wound. And found that feces/urine had seeped into the wound. The patient will have wound pain from rubbing and rubbing the wound every time the wound is dressed. Therefore, the method of dressing the wound was changed proactively by using a syringe to douche the wound and inject saline (0.9%NSS; normal saline) to clean the wound instead of wiping. The dead tissue was removed using sharp debridement at regular intervals after 39 days of the original wound dressing. It was found that the wound had much dead tissue reduced. However, the trend in the size of the wound did not decrease. Together with the results of the wound culture examination, no infection was found. Therefore, the method of dressing the wound was changed. A new way to treat wounds is to make the wound using a vacuum (Negative pressure wound therapy). A syringe is used to clean the wound. After that, use a sponge (open cell foam dressing) and place it on the wound, then cover the sponge with wound dressing material. Close each edge of the skin 3-5 centimeters away from the sponge, then connect the end of the suction hose to a suction wall machine, using suction power with a constant pressure of 120mmHg continuously. And change the wound every three days. The results of this new wound dressing method showed that the wound's size decreased rapidly. The wound cavity became noticeably shallower. The number of wound dressings has decreased. It helps reduce the workload and the working time of personnel dressing wounds. Reduce the cost of dressing wounds. Reduce discomfort from wound dressings for patients. Application of the nursing process to solve health problems. Pressure injury management from the case study example, it was found that the patient was significantly impacted by the non-healing wound and infection. The prolonged dressing process, frequent contamination, and associated material costs not only caused physical discomfort but also psychological distress. The items were analyzed as follows:
The wound healing process has 3 phases: 1) the inflammatory phase (inflammatory phase) and 2) The phase where cells divide. (proliferative phase) 3) Adjustment phase (remodeling phase). Usually, all 3 phases of the process will take at most 3-4 weeks. However, if the wound does not tend to heal in that period, it is called a chronic wound (chronic wound) [10]. Therefore, wound care must be taken care of, and wound dressing methods must be adjusted to promote healing. The causes affecting the wound healing process in this case study patient are as follows: Common causes include infection, irritation of granulation tissue, malnutrition, and pain. Malnutrition and pain have been addressed. But there is also the problem of infection. In the bloodstream, there is infection in pressure sores. Therefore, the factors affecting wound healing in this patient are contamination and infection of the wound. And irritation of new tissue (granulation tissue)
When the wound is infected or contaminated with germs, it is necessary to clean the wound and apply a material that destroys or inhibits the growth of microorganisms. It can prevent infection and treat infected wounds. In this case study, Povidone iodine is a substance that destroys or inhibits the growth of microorganisms, and its effectiveness is a key factor in its use. It can prevent infection and heal infected wounds [9]. It is effective against bacteria, fungi, protozoa, and viruses. Its mechanism involves changing iodine into povidone-H+ ions or changing from a complex state to a polyelectrolyte to bind to the negative charge of the cell wall. Iodine enters the germs by penetrating the cell wall and interfering with the enzymes used to create proteins for the germs' cell division. As a result, the pathogen stops cell division, cannot reproduce, and eventually dies [11]. and there are no reports of toxicity. Alternatively, for tissue irritation from free iodine, those who are allergic to iodine will have a red rash-corrected by stopping the drug immediately and providing medical treatment until symptoms improve [12].
Cleaning the wound each time may irritate the wound surface of the granulation tissue, causing it to peel off easily. from loose adhesion. This depends on the intensity of the rubbing when treating the wound. Therefore, it's crucial to avoid vigorous scrubbing, as it can lead to unintended consequences. However, an appropriate amount of dirt and bacteria must be removed. On the wound surface, the solution used to dress the wound must not irritate or be toxic to regenerating tissue cells, such as normal saline (NSS) [12]. Therefore, the patient in this case study also cleaned the wound. The method of douching and using liquid to treat wounds is normal saline (NSS).
This is because the patient's wound is large and deep, and he is unable to help himself. Restricted movement: Each wound dressing requires more than one person to help turn the body on its side and dress the wound, including a large wound. This makes the time needed for each wound to be treated long. Including when excretion stains the wound. More wounds will need to be done than planned. Moreover, personnel are required to help change clothes for 2-3 patients.
In each wound dressing, there is a cost of dressing the wound of 746 baht, and the patient in this case study has his wound dressed two times a day, accounting for an average cost of 1,492 baht. It's crucial to prevent situations that could lead to additional wound dressings, as the cost will increase significantly due to fecal contamination/ urine, underscoring the urgency of prevention.
Nursing planning
Nursing diagnosis number 1: The pressure injury on the coccyx is infected.
Supporting information: The patient presented with a severe grade 4 pressure injury on the coccyx. Wound culture results revealed the presence of highly resistant bacteria, Acinetobacter baumannii (CRAB MDR), and Enterococcus faecium.
Objective: Our primary goal is to ensure the patient's safety from infected pressure injury. The pressure injury must not become infected.
Evaluation criteria: The wound was clean, odor-free, and most importantly, free from any signs of infection. Culture results post-nursing and treatment confirmed the absence of any infection.
Nursing care
Make a wound by wiping the wound clean with cotton and gauze moistened with saline (NSS; normal saline). Wipe the wound and then use gauze moistened with povidone-iodine, which is a substance that destroys or inhibits the growth of microorganisms. It can prevent infection and treat infected wounds Put in the wound and cover the wound with a large gauze (Gamgee). The wound is dressed two times a day, but the wound will be changed when it is found that feces/urine has penetrated the wound. The patient will experience pain from rubbing and rubbing the wound every time it is treated. Therefore, the method of dressing the wound has been changed by using a syringe to douche the wound and inject saline (0.9%NSS; normal saline) to clean the wound instead. Mopping Necrotic tissue is removed using sharp debridement at regular intervals. Repeat wound cultures are followed up.
Nursing evaluation: The wound has no dead tissue and no bad smell. Pressure sores are cultured periodically. After 39 days of dressing the wound, the culture results from the pressure sore did not find any infection.
Nursing diagnosis number 2: There is a grade 4 pressure injury from a complication from lying down for a long time.
Supporting information: who is currently bedridden, is presenting with a grade 4 pressure injury on the coccyx.
Objective: experiencing progress in the healing of their pressure injuries and is pleased with the wound dressing process.
Evaluation criteria: the size and depth of the wound decreased. The rate of recovery has increased.
Nursing care
After 39 days of dressing the wound using the same method, it was found that the wound had much dead tissue reduced. However, the trend of wound size did not decrease. Together with the results of the wound culture examination, no infection was found. Therefore, the method of dressing the wound was changed. It is a method of making the wound using a vacuum (Negative pressure wound therapy). A syringe is used to clean the wound. After that, place a sponge (open cell foam dressing) on the wound and cover the sponge with wound dressing. Close each edge of the skin 3-5 centimeters away from the sponge, then connect the end of the suction hose to a suction wall machine, using suction power with a constant pressure of 120 mmHg continuously, and change the wound every three days. Follow up and evaluate wound healing every seven days.
Nursing evaluation: The wound has significantly decreased in size and depth, indicating a positive trend in the patient's recovery.
CONCLUSIONS
Pressure injuries are still a problem that requires attention to dressing the wound if the wound tends to get worse. The wound-healing process does not follow as it should. The wound care method must be changed. By considering essential factors involved with wound healing, Dressing the wound using a vacuum consists of making a wound using a closed system with a pressure lower than atmospheric pressure. The study obtained from this case study patient found that complex wounds can be treated more easily. Reduce the time and number of wound dressings. Reduce the number of personnel to treat wounds, reduce costs, and make wounds heal faster. Even though the wound had not completely healed in this patient, there is a trend of increasing wound healing rates.
DISCUSSIONS
Wound management in this case study patient Began with a problem of pressure injury infection. The current method of dressing the wound, however, proves to be inefficient when the wound is not infected, leading to poor healing outcomes, wasted time, and increased workload. This approach also escalates the overall cost of wound care. To address these issues, a new method of wound management has been introduced to promote wound healing, reduce pain and suffering from frequent dressing changes, lessen the burden on healthcare personnel, and cut down on wound dressing costs.
How to dress a wound
Wound dressings focus on preventing tissue regeneration from injury and damage. Using irrigation with 0.9% normal saline (NSS) and accelerating the wound healing process by using vacuum (Negative pressure wound therapy), the details are as follows:
Irrigations with 0.9% normal saline (NSS), a size 19 needle and a 35-milliliter syringe will rinse with a pressure of approximately 4-15 pounds per square inch. This effective method prevents injury to the regenerating tissue, as no abrasive force is applied directly to the wound surface. In this case study patient, the wound is large, with no dead tissue, eliminating the need for high pressure. Therefore, a 50 ml syringe, not a needle, is used to clean the wound, ensuring an effective cleaning process.
Negative pressure wound therapy
Vacuum dressing helps keep the wound moisturized at an appropriate level. Reduces the amount of secretions and bacteria in the wound. The mechanical force pulls surrounding cells to grow into the wound. Including increasing the growth of new blood vessels to feed the wound. The optimum vacuum pressure is 125 mmHg [13]. Results from new wound management in this case study patient. It was found that patient and personnel satisfaction was improved. Expenses and the size of the wound.
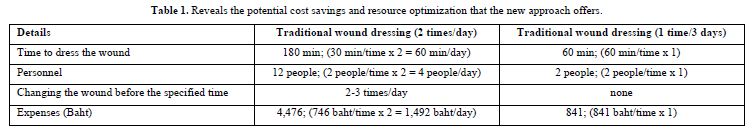
Satisfaction aspect
From the patient's perspective, the new wound care approach has significantly improved their quality of life. They express gratitude after each treatment, reporting that the wound is less painful and allowing them to sleep better. The fear of the wound worsening has also diminished, creating a more positive patient experience. From the personnel's viewpoint, the new system of assigning specific nurses to the patient's ward has proven to be highly efficient. It has significantly reduced the workload and time spent on wound dressings, allowing for more tasks to be accomplished. The patient's wound has shown rapid improvement, underscoring the effectiveness of this approach. When it comes to costs, time, and workforce, the comparison between traditional and new wound treatments is significant. A detailed breakdown, as provided in the table, reveals the potential cost savings and resource optimization that the new approach offers (Table 1).
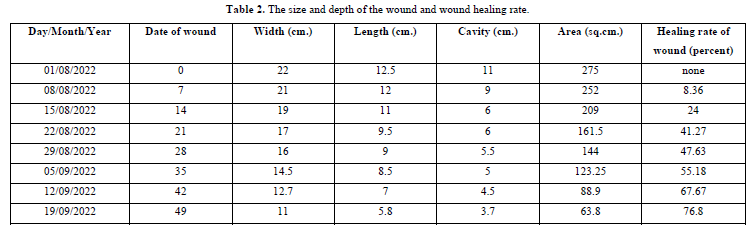
The Table 2 shows the size and depth of the wound. Wound healing rate (Counting from the start of the vacuum wound dressing)
Calculate the wound area: width x length.
Calculate the wound healing rate using the formula:
(first day area - compared date area) /first day area x 100
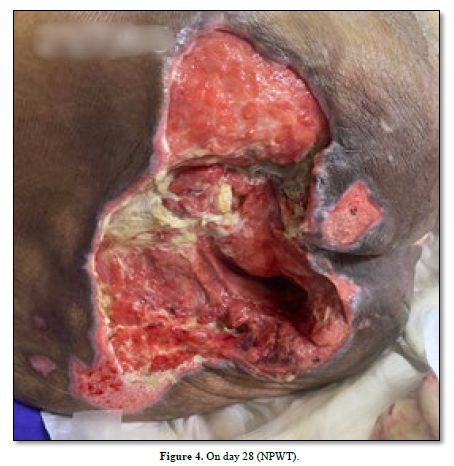
Picture of the wound healing progress of this case study patient (Figures 1-5).




SUGGESTIONS
No Files Found
Share Your Publication :